
Multiple scientific investigation and evidence reveals salt usage levels below 8g daily is associated with health risk factors as discussed below and the article here Salt and Our Health by Morton Satin
The case for consuming at least eight grams daily of salt - preferably unrefined Salt (Such as Celtic Salt)
Multiple research has found that there is an typical amount of salt consumption across the planet in peoples who have free access to salt, and that the average quantity consumed is close to an amount that has also been found in multiple studies to collate with the least amount of diseases such as cardio-vascular, diabetes and syndrome X - including obesity. This average quantity is in the region of ten grams daily of salt consumed. Contrary to main stream media and medical industry disinformation, the less salt that is consumed below this level the greater the disease incidence, specifically cardio-vascular and diabetes. Quantities consumed in excess of about 15 or 17 grams daily (Although this research is less clear and generally is looking at a mixture of refined and unrefined salt grouped together in the statistics consumption) are indicative of increasing disease.
Because salt is essential to good health, the human body is hard-wired with an innate salt appetite. Around the world, population salt intakes vary somewhat, but nearly all fall within what eminent medical researcher Bjørn Folkow termed the "hygienic safety range” of sodium intake, between 6 gram salt daily and 14.6 gram salt daily.
More studies Vindicating salt
SOURCE:http://www.saltinstitute.org/Issues-in-focus/Food-salt-health/Salt-and-cardiovascular-health
1985. A ten-year study of nearly eight thousand Hawaiian Japanese men concluded: "No relation was found between salt intake and the incidence of stroke."
1995. An eight-year study of a New York City hypertensive population stratified for sodium intake levels found those on low-salt diets had more than four times as many heart attacks as those on normal-sodium diets—the exact opposite of what the "salt hypothesis” would have predicted.
1997. An analysis by NHLBI’s Dr. Cutler of the first six years’ data from the MRFIT database documented no health outcomes benefits of lower-sodium diets.
1997. A ten-year follow-up study to the huge Scottish Heart Health Study found no improved health outcomes for those on low-salt diets.
1998. An analysis of the health outcomes over twenty years from those in the massive U.S. National Health and Nutrition Examination Survey (NHANES I) documented a 20 percent greater incidence of heart attacks among those on low-salt diets compared to normal-salt diets.
1998. A health outcomes study in Finland, reported to the American Heart Association that no health benefits could be identified and concluded "…our results do not support the recommendations for entire populations to reduce dietary sodium intake to prevent coronary heart disease.”
1999. A further analysis of the MRFIT database, this time using fourteen years’ data, confirmed no improved health benefit from low-sodium diets. Its author conceded that there is "no relationship observed between dietary sodium and mortality."
2002. In September 2002, the prestigious Cochrane Collaboration produced the latest and highest-quality meta-analysis of clinical trials. It was published in the British Medical Journaland confirmed earlier meta-analyses' conclusions that significant salt reduction would lead to very small blood pressure changes in sensitive populations and no health benefits.
2003. In June 2003, Dutch researchers using a massive database in Rotterdam concluded that, "variations in dietary sodium and potassium within the range commonly observed in Westernized societies have no material effect on the occurrence of cardiovascular events and mortality at old age."
2006. A March 2006 analysis of the federal NHANES II database in The American Journal of Medicinefound a 37 percent higher cardiovascular mortality rate for low-sodium dieters.
2007. A February 2007 article reported in the International Journal of Epidemiology described a study of over forty thousand Japanese over seven years and found "the Japanese dietary pattern was associated with a decreased risk of CVD mortality, despite its relation to sodium intake and hypertension."
2007. An October 2007 analysis of a large Dutch database published in the European Journal of Epidemiology documented no benefit of low-salt diets in reducing stroke or heart attack incidence nor lowering death rates.
2008. A May 2008 examination of NHANES II (the largest U.S. federal database of nutrition and health) published in the Journal of General Internal Medicine confirmed two earlier studies of earlier NHANES surveys that there is no health benefit (CVD or all-cause mortality) for those on low-sodium diets.
And more In a recent study, published in the Journal of the American Medical Association (JAMA), 31 researchers found moderate salt intake to be associated with the lowest risk of cardiovascular events whereas low intakes, equivalent to less than 7.5 gram salt or 3 slightly rounded common domestic teaspoons daily (1.5 medicinal heaped teaspoons of salt per day) , were associated with an increased risk of cardiovascular death and hospitalization for congestive heart failure, higher intakes of more than 17.5 gram or approximately 6 x 3 ml teaspoons (3.5 level medicinal spoons) of salt per day, were associated with an increased risk of stroke, heart attack and other cardiovascular events. Once again, a J-shaped curve appeared to describe the dose-response relationship.
Extracts from Salt and Our Health by Morton Satin PhD
http://www.westonaprice.org/vitamins-and-minerals/salt-and-our-health
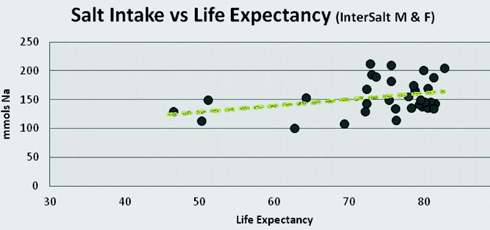
When average life expectancy in various countries is plotted against the average saltintake in those countries, it is clear that the higher the saltconsumption, the longerthe life expectancy. (See Figure 3.) While no cause-and-effect relationship between sodium intake and lifespan is implied, the data clearly demonstrate the compatibility between life expectancy and the associated levels of sodium intake. (e.g. 200 mmols Na means 11.8 grams of salt consumed on average each day)
Public Pressure To Reduce Salt
In the late 1980s, in response to the notion that sodium had a major impact on a population's blood pressure, an international study (Inter salt) was carried out to determine the impact of salt consumption on blood pressure.7 As it turned out, the per capita consumption of sodium in the majority of countries ranged between 7.7 to 12.4 grams salt daily. (Example 9 grams of salt is contained in 3 x 3ml teaspoons of unrefined salt) The results indicated that there was no clear pattern between the level of salt intake and blood pressure.
However, there were four populations among the fifty-two groups that showed very low salt intakes and far lower than average blood pressures. (Pathologically low!) The lowest consumption population in this group was the primitive Yanomami Indians, who live in the Brazilian rain forest. Normally, data points that are very far from the rest of the pattern are referred to as outliers and are generally omitted from the analysis. In this case, the outliers were included and a line drawn from them to the rest of the population in order to show that a pattern relating salt consumption to blood pressure did exist. (See Figure 1 below) The Yanomami are characterized as a small stature, high mortality and high fertility population with a low life expectancy. The Yanomami are described in the ethnographic literature as an aggressive and violence-prone people. It is also interesting to note that despite their long history of evolution in a salt-limited rainforest environment, they have never acclimatized to low sodium intake and have chronically high levels of plasma renin. (An indication of salt deficiency- stress ) Nevertheless, the inclusion of the Yanomami data in the formal Inter salt analysis, however misguided, initiated the latest round of salt restriction efforts.
Ed: Low salt consumption has been related by Professor Jacques De Langre (Seasalt's Hidden Powers) as resulting in a kind of madness that occurred in the middle ages when certain salt marshes became drained and little salt was available to the population. Low salt intake and low blood pressure is a problem, especially amongst vegetarians and results in poor mental composure and function, along with a host of other complaints. The fact that the Yanomami Indians where used as a justification for low salt consumption, beggars comprehension! Furthermore the relationship between B.P and life expectancy has not been proven! The salt restriction agenda is a genocidal program of indoctrination!
Figure 1. InterSaltStudy
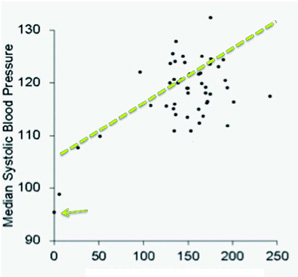
Figures on bottom line are 0 to 250 mmols of sodium consumed daily. 200 mmols Na means 11.8 grams of salt consumed on average each day. The general consensus is that blood systolic pressures below 100 are indicative of insufficient blood pressure for optimum function and health, and average blood pressures up to or even beyond 130 systolic are considered in a normal adult range
End of Extracts from Salt and Our Health by Morton Satin PhD http://www.westonaprice.org/vitamins-and-minerals/salt-and-our-health
Regardless of the evidence, we now must face a certain reality resulting from the two decades long campaign to reduce salt. Because the Dietary Reference Intakes for salt were promulgated by the Institute of Medicine, they were immediately adopted without question by most public health agencies around the world. This position, repeated and amplified by an uncritical press influenced the food industry to consider salt reduction strategies very seriously, not because there was genuine concern for the impact of salt on health, but for two commercial considerations. The first was the concern related to public pressure as the food industry did not want to be perceived as purveyors of unhealthy products. Second, reduced salt product formulations had the potential to become new "low salt” varieties that might capture additional market share.
Extracts from It’s Your RAS ! Morton Satin, Salt Institute www.saltinstitute.org
The Renin - Angiotens in System or RAS, is Mother Nature's way to make up for inadequate salt consumption. When any one of our body’s sensory mechanisms detects that we’re not eating enough salt, the RAS kicks in to make the kidney re-absorb sodium and water back into the blood1.
"This complex hormonal chain reaction, perfected through millions of years of biological evolution,is critical for maintaining balance in our circulatory system… Unfortunately,although the RAS helps us make up for too little salt consumption,it does so at a heavy cost to our health. Elevated RAS levels cause metabolic syndrome 2, insulin resistance3, cardio vascular disease 4, and a host of other serious conditions 5,6,7.There is no longer any doubt that an elevated RAS is a very serious risk factor for overall health.So anyone who cuts salt to reduce blood pressure ends up increasing their risk for other diseases”
Once our salt intake falls below 9 grams of salt a day, the body reacts by producing high levels of renin in kick start the RAS chain reaction to conserve s odium. Its nature’s way to make up for an inadequate salt consumption. Nine grams of salt, is close to the average American, European and other countries consumption9. (This is an interesting example of the ‘wisdom of the body,’10 the idea that our body’s physiology is the best authority on determining our personal needs.) This average level of salt consumption is sufficient to prevent any spike in RAS activity. However, the Dietary Guidelines for Americans recommends that we drop our consumption down to 6 gram s of salt a day. At this level, the renin begins to rise rapidly. To make matters worse, the 2010 issue of the Dietary Guidelines recommends 3.8 gram s of salt daily for more than half the American population. At this red line level, renin spikes up dramatically. Yet, in the Dietary Recommended Intakes, the original publication upon which all the supposed salt reduction benefit are based, nature’s response to reduced sodium was deliberately ignored in order to promote a salt reduction agenda11. And it is this flawed publication that continues to drive the s alt reduction agenda today! (End of extract)
More about the benefits of unrefined Celtic Salt
It is worth re-iterating here than for persons with high blood pressure, the introduction of unrefined salt (Such as Celtic Salt with its high trace mineral composition) results almost invariably in a reduction of blood pressure.
Salt has been treasured throughout time by both man and animals alike; it is a vital substance for maintaining health. We constantly hear bad press about salt, and indeed refined salt is inferior in health befits to unrefined salt, we need natural salts for our bodies to function properly. "Salt" is mainly sodium chloride; Sodium is an essential nutrient; the body cannot manufacture sodium, yet is it is required for life itself. Chloride is also vital for optimum health; it preserves the acid-base balance in the body, aids potassium absorption, supplies the essence of digestive stomach acid, and enhances the ability of the blood to carry carbon dioxide from respiring tissues to the lungs. .
Every cell in our body is bathed in a clear fluid called extra cellular fluid,similar to sweat. The amniotic fluid that surrounds the fetus in the womb is of similar composition.The closest to this natural body fluid found in nature is sea water.Our blood, sweat and bones, contains salt which makes it easy to see why pure, unrefined,salt is essential for good health.This takes on further meaning when we consider that the life forms we evolved from were single celled, sea organisms. It is worth noting that sea creatures die if exposed to a mixture of refined salt and water.
Unrefined Celtic Salt has considerably more trace minerals than standard sea or rock salts and is that is revealed by its taste and the improvement in flavor of food. Celtic Ocean Sea Salt is dried using a process first started well over 900 years ago. This drying process in the natural elements of the West Brittany coast, charges the salt with natural energy. No metal ever comes into contact with the salt. The coast of Brittany, France is considered to have the best mineral content of any seawater in the world. Clickhere for Celtic Salt Information
Examples of how to add salt to your diet.
As someone who does not purchase processed food or eat meat, and had been influenced by the low salt lobby, I find it almost impossible to consume at least 10 grams of unrefined salt daily just by adding to food. So to obtain my daily salt needs I add a gram of salt to every cup of tea or coffee I drink, and soon adapted to the new taste. I also add some salt to some of the water I drink. I also add salt to foods I would normally not such as fruits and find the taste is improved. Ironically it tends to be health conscious people that do not eat much processed food and who eat plenty of fruit and vegetables and little meat that tend to be the most salt deficient, especially since a quality diet tends to be relatively higher in potassium, the counterbalancing mineral to sodium. Since dramatically increasing my salt consumption, energy and other aspects of health have improved and monitoring Blood pressure proves there is no connection to excessive blood pressure to moderate salt consumption in the region of 10 to 15 grams a day. However, low salt consumption i.e. below about 6 gram a day is often associated with excessively low blood pressure, i.e. systolic readings below 100. Low blood pressure can result in insufficient oxygen and nutrients getting into the cells resulting in below par energy and health. Raising your salt intake in these cases will usually result in a normalization of blood pressure to provide more robust health.
Prior to refrigeration a fair proportion of the diet was preserved using salt. Civilizations flourished in areas where salt was freely available as sufficient salt is essential for robust health and full mental capacity. Since the introduction of refrigeration many individuals have become salt impoverished.
For a collection of articles on salt from the Salt Institute see:
http://www.saltinstitute.org/News-events-media/Salt-Institute-Press-Releases-and-Statements
A further article of interest from the Weston A Price foundation can be read here The Salt of The Earth by Sally Fallon Morell
Recommended reading : Sea Salt's Hidden Powers Dr. Jacques de Langre (Amazon UK link) California Biochemist Dr. Jacques de Langre studied the health benefits of salt for over 30 years. He gained a Ph.D. in biochemistry from the University of Brussels.
Also recommended reading is Salt Your Way To Health by David Brownstein M.D. (This book details some case histories)
References
1 Wikipedia. The Renin-Angiotensin System. Available at: http://en.wikipedia.org/wiki/Reninangiotensin_system
2 Alderman MH, Madhavan S, Ooi WL, Cohen H, Sealey JE, Laragh JH. Association of the renin sodium profile with the risk of myocardial infarction in patients with hypertension. 1991; N Engl J Med 324:1098–1104.
3 Bernstein AM,WillettWC. Trends in 24-h urinary sodium excretion in the United States, 1957–2003: a systematic review. Am J Clin Nutr 2011;92: 1172–80.
4 Cannon,WB. The Wisdom of the Body. 1932,W.W.Norton & Co. New York.
5 National Academy of Sciences. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. 2004; page 282.
6 Wang CH, Li F, Takahashi N. The renin angiotensin system and the metabolic syndrome. Open Hypertens J. 2010;3:1-13.
7 Liu Z. The renin-angiotensin system and insulin resistance. Curr Diab Rep. 2007 Feb;7(1):34-42.
8 Verma S, Gupta M, Holmes DT et al. Plasma renin activity predicts cardiovascular mortality in the Heart Outcomes Prevention Evaluation (HOPE) study. Eur Heart J. 2011; (first published online March 17, 2011 doi:10.1093/eurheartj/ehr066).
9 Peti-Peterdi J, Kang JJ, Toma, I. Activation of the renal renin–angiotensin system in diabetes—new concepts. Nephrol. Dial. Transplant. 2008; 23 (10): 3047-3049.
10 Inaba S, Iwai M, Furuno M, et al. Continuous activation of renin-angiotensin system impairs cognitive function in renin/angiotensinogen transgenic mice. Hypertension. 2009 Feb;53(2):356-62. Epub 2008 Dec 1.
11 Takahashi N, Li F, Hua K, et al. Increased energy expenditure, dietary fat wasting and resistance to diet-induced obesity in mice lacking renin. Cell Metab. 2007 December; 6(6):506–512.